A major IT failure that caused weeks of problems at four major Greater Manchester hospitals will cost the NHS more than £650k, it has been revealed.
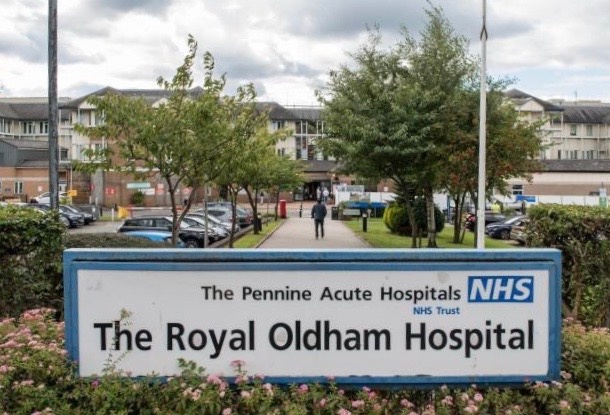
The issue, which began on 17 May, impacted most clinical systems in Fairfield General, Rochdale Infirmary, the Royal Oldham Hospital and North Manchester General Hospital.
Thousands of patients were affected when IT problems caused chaos with services including electronic prescribing, viewing patients’ medical records and finding test results, and forced staff to move back to a paper system.
A report to a health scrutiny board this week states that around 1,000 appointments and procedures were cancelled, with the biggest impact felt in specialities such as treating eye conditions.
The IT failures prompted critical incidents and business continuity incidents to be declared across the hospitals.
A report presented to Oldham’s health scrutiny board on Tuesday night by the Northern Care Alliance NHS foundation trust states that the cost of ‘managing and recovering’ from the impact of the outage is estimated at £675,000.
Staff had to shift to handwriting documents and using dictaphones during the failure. Not all of the dictaphone records have yet been added into patients’ records, and the communication disruptions may require patients to have further hospital attendances and diagnostic checks, the report states.
Of staff who responded to a ‘de-brief’ form across the health organisations affected, 67 per cent said that patient safety had been ‘compromised’ during the IT failure.
During the period of the outage there were 327 incidents of ‘low harm’ reported across the hospitals, most of which related to medications and missed drug dosage, documentation and IT security.
There were two incidents of ‘moderate harm’ involving a medication error and a surgery related incident. Additionally one serious incident was reported which related to end of life care, in which a referral was made to the coroner containing ‘incorrect patient demographics’.
“Internal investigations are underway for all moderate and above incidents of harm in line with trust incident management policy,” the report states.
“It is anticipated the current number of incidents reported may increase over the next few weeks or months.”
The outages were caused by a previously unknown ‘inherent software defect. This had been ‘triggered by a very specific set of conditions’ – including a server being disconnected for routine maintenance purposes for less than five minutes, combined with the outcomes of nightly backups running while the server was disconnected.
The disconnection ‘would not normally cause any adverse impact’ and the nightly backups are also part of the ‘core design’ of the system.
David Jago, chief officer at the NCA, said: “I can now happily report to members that that defect has been rectified and can not now happen again through the installation of a version three element of software to rectify that. So I can report with confidence that that will not be experienced again within the north east sector.”
He told the meting they had initially believed they were dealing with a ‘low level resilience issue’ but later realised it was more serious.
When asked by the Local Democracy Reporting Service Mr Jago would not confirm whether the trust would be seeking compensation from its IT and software suppliers for the outage.
He told the meeting: “We’re working with our commercial partners in terms of understanding those complexities of costs incurred and we’ll I’m sure come to a successful conclusion in those discussions.”
Since the incident he said they had been working with NHS Digital which had been ‘really impressed by our learning, our response time’. Mr Jago added they had been undertaking ongoing audits around clinical safety.
Mike Barker, formerly the accountable officer for Oldham’s clinical commissioning group and now ‘place lead’ for the Greater Manchester Integrated Care System, said: “This was a very, very challenging couple of weeks for the hospital, certainly for the staff who have been remarkable.”


 Police Appeal For Help In Finding Missing Man with Dementia
Police Appeal For Help In Finding Missing Man with Dementia
 Spindles Shopping Centre Wins Award
Spindles Shopping Centre Wins Award
 Update on Wrigley Head Solar Farm
Update on Wrigley Head Solar Farm
 Crime is Down And Solve Rates Are Up - GMP
Crime is Down And Solve Rates Are Up - GMP